The Kidney Clinic
Chronic Kidney Disease (CKD)
Chronic Kidney Disease (CKD) is a long-term condition characterized by a gradual decline in kidney function over time. The kidneys, which are crucial for filtering waste products and excess fluids from the blood, become less efficient at performing these functions as CKD progresses. This decline can eventually lead to kidney failure.
Causes and Risk Factors
CKD can result from a variety of underlying conditions, including:
- Diabetes: High blood sugar levels can damage blood vessels in the kidneys.
- Hypertension (High Blood Pressure): Elevated blood pressure can damage kidney blood vessels over time.
- Glomerulonephritis: Inflammation of the kidney’s filtering units (glomeruli).
- Polycystic Kidney Disease: A genetic disorder characterized by the growth of cysts in the kidneys.
- Prolonged Use of Certain Medications: Some medications can contribute to kidney damage.
Symptoms
In the early stages, CKD may not present noticeable symptoms. As the disease progresses, symptoms may include:
- Fatigue: Feeling unusually tired or weak.
- Swelling: Fluid retention causing swelling in the legs, ankles, or face.
- Urinary Changes: Changes in frequency, volume, or appearance of urine.
- Shortness of Breath: Fluid buildup in the lungs can lead to breathing difficulties.
- Nausea and Vomiting: Accumulation of waste products in the blood can cause gastrointestinal issues.
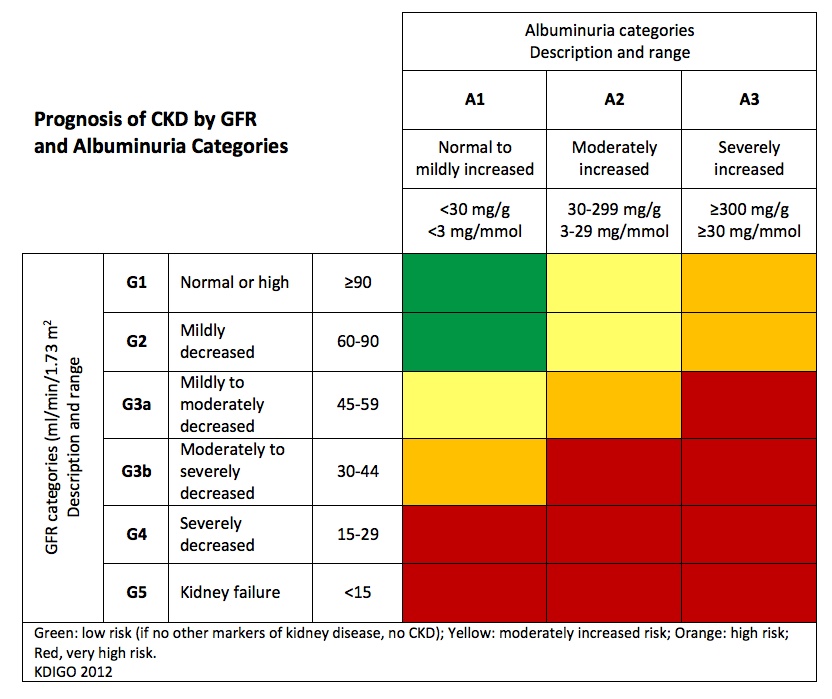
Stages of CKD
CKD is classified into five stages, based on the level of kidney function, measured as the Glomerular Filtration Rate (GFR):
- Stage 1: Mild kidney damage with normal or high GFR (≥90 ml/min).
- Stage 2: Mild kidney damage with a decreased GFR (60-89 ml/min).
- Stage 3: Moderate kidney damage (30-59 ml/min).
- Stage 4: Severe kidney damage (15-29 ml/min).
- Stage 5: Kidney failure (GFR <15 ml/min), often requiring dialysis or a kidney transplant.
Diagnosis
CKD is diagnosed through a combination of:
- Blood Tests: Measuring kidney function markers such as serum creatinine and blood urea nitrogen (BUN).
- Urinalysis: Testing urine for protein, blood, or other abnormalities.
- Imaging Studies: Ultrasound or CT scans to assess kidney size and structure.
- Kidney Biopsy: In some cases, a biopsy may be performed to determine the cause of kidney damage.
Treatment and Management
While CKD is a progressive condition without a cure, its progression can be slowed, and complications managed through various treatments:
Medications:
- Blood Pressure Control: Medications such as ACE inhibitors or ARBs can help protect kidney function.
- Blood Sugar Control: For diabetic patients, medications to maintain blood glucose levels within target ranges.
- Phosphate Binders: To manage elevated phosphate levels.
Lifestyle Changes:
- Dietary Modifications: Reducing salt, potassium, and phosphorus intake, and managing protein consumption.
- Exercise: Regular physical activity to help manage blood pressure and weight.
- Smoking Cessation: Stopping smoking to reduce further kidney damage.
Monitoring and Managing Complications:
- Anemia Management: Use of erythropoiesis-stimulating agents or iron supplements.
- Bone Health: Treatments for mineral and bone disorders related to CKD.
Dialysis:
- Hemodialysis: A procedure where a machine filters waste and excess fluid from the blood when the kidneys are no longer able to perform this function.
- Peritoneal Dialysis: A process where the abdominal cavity is used to filter waste from the blood.
Kidney Transplant:
- A surgical procedure where a healthy kidney from a donor is transplanted into the patient. It is a viable option for eligible patients with end-stage kidney disease.
Regular Monitoring
Patients with CKD require regular follow-ups to monitor kidney function, manage complications, and adjust treatments as needed. Early detection and proactive management are key to maintaining kidney health and preventing progression.
